Background: Complications of sickle cell disease (SCD), including vaso-occlusive crises (VOC), usually require emergency room visits or even hospitalization for management. Outpatient treatment programs have been developed for management of VOC, however the literature is limited as to the efficacy of these models. Previously, patients in Edmonton, Canada followed by the Hemoglobinopathy Clinic would have to present to the emergency department (ED) for assessment of and management of VOC. Since 2019, patients experiencing early VOC symptoms were able to present to the Medical Outpatient Unit (MOU), an infusion clinic shared with other benign and malignant hematology conditions, to be assessed and receive treatment. This study retrospectively evaluated the outcomes of this treatment strategy.
Hypothesis: Outpatient management of VOC is an effective way to assess patients and provide appropriate treatment, thereby reducing the frequency of ED presentations for SCD patients.
Methods: Patients were able to schedule their own appointments and were encouraged to present early before they developed severe symptoms. They would be assessed by a nurse, who could then release orders from their personalized pain plan, which is a standing set of orders from an SCD clinic physician. Examples of orders include intravenous fluids and pain medications. Based on the severity of symptoms, patients could also be referred to the ED or for assessment by a physician or nurse practitioner.
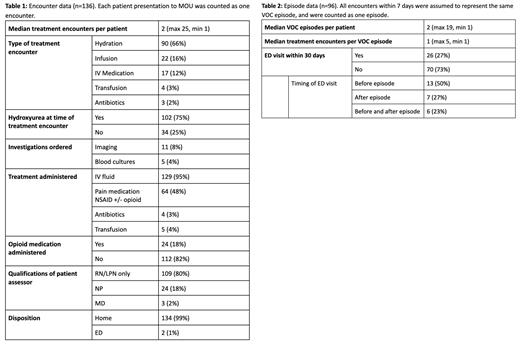
Chart review of patients aged 18 years or older with SCD followed by the Edmonton Hemoglobinopathy Clinic and who presented to MOU from November 2019 to December 2022 for management of VOC was completed. Information gathered included if the patient was on hydroxyurea at the time, investigations ordered, treatments administered, if NP or physician assessment was required, and disposition following the encounter. Encounters within 7 days were counted as one episode and assumed to be the same VOC event. Visits to ED for this cohort were counted and compared to the number of ED visits from 2016 to 2018.
Results: 26 SCD patients had at least one MOU encounter for VOC or prophylaxis resulting in a total of 136 encounters (median 2, maximum 25). These accounted for 96 separate episodes of VOC (median 2, maximum 19), with a median of 1 encounter to MOU per episode (maximum 5). Patient demographics had a mean age of 32 years as of the beginning of the study (maximum 65, minimum 16) with 14 males (54%) and 12 females (46%). Patient diagnoses included 10 with HbSS (38%), 12 with HbSC (46%), 3 with HbSD (12%), and 1 with HbSB° (4%). 21 of 26 patients (81%) were on hydroxyurea at some point during this time period. IV fluids were administered in 129 encounters (95%), and pain medications were given in 64 encounters (47%), with opioid medications being given in 24 encounters (18%). 109 encounters had assessment by a nurse only (80%), while 24 were also assessed by a nurse practitioner (18%) and only 3 required assessment by a physician (2%). Patients were discharged home in 134 of 136 encounters (99%), with only 2 encounters resulting in assessment in ED. 70 of 96 episodes of VOC treated in MOU did not have presentation to ED within 30 days (73%). Total ED visits for this cohort decreased from 59 in 2016-2018 to 38 during the time of this study.
Conclusion: Treatment of VOC in an outpatient setting was effective for assessment and treatment and decreased ED visits in our cohort. While retrospective, these results suggest outpatient treatment of VOC can be completed safely and efficiently in a shared infusion unit and may be generalized to other centres with outpatient IV infusion programs.
Disclosures
No relevant conflicts of interest to declare.